Mental Health and Violence: Not a Clear-Cut Relationship

Most people with mental health issues are not prone to violence
Image by StoryMD
— By Barra O Suilleabhain, StoryMD Staff Writer
"Downtown stabbing suspect had a long history of mental health issues."
Headlines like this are a dime a dozen and satisfy the widespread public perception that mentally ill people are prone to violence. News reports, films, TV shows, and books go a long way toward shaping our views of other people and groups — whether we're conscious of it or not — and those with mental health disorders have long been a convenient dumping ground for stigmatization, derision, and scapegoating.
"Unpredictable, dangerous, and unhinged" is the general sentiment that drives this discrimination, and the result is a cohort of vulnerable individuals being maligned by society. From here, they are more likely to find themselves living in poverty in rough neighborhoods, with poor employment opportunities and access to services.
Writing off violent acts by individuals with a background of mental health issues as a product of their illness is a convenient way to wash our hands of the issue. But if you dig deeper, the data doesn't stack up: the majority of people with a mental health condition are not prone to violence, and other factors common to broader society are much bigger drivers of the issue.
This isn't to say that psychiatric influences play no role whatsoever; the point is that their contributions are overblown because it fits sensationalized headlines that confirm our preconceived narrative.
When a person with a psychiatric condition does commit violence, it is in many cases intertwined with other factors that catalyze the situation. Substance abuse issues, traumatic childhood experiences, and environmental factors are often critical in what sends someone over the edge.
"If a person has a severe mental illness, [they] may have other risk factors for violent behavior," said Eric B. Elbogen, a psychologist and professor of psychiatry and behavioral science at Duke University School of Medicine, to the American Psychological Association.
"So, it may not be mental illness that is driving the violence at all, but rather factors like having been abused as a child, being unemployed, or living in a high-crime neighborhood."
The impact of discrimination
Understanding these issues is important not only because it will help us to help these individuals to receive better treatment (along with better support for families and communities), but also because we need to combat misconceptions that foster unwarranted discrimination.
Incidents of mass violence are often blamed on mental illnesses, and the same goes for general community violence. But the reality is that it isn't so simple, and research shows there are serious costs to these attitudes: people are more likely to support forced legal action and coercive treatment for those with mental health conditions if violence is perceived to be at hand. This association has also been used to justify bullying and other forms of victimization.
Stigma and discrimination can pollute all areas of a person's life, from employment and housing to relationships and more. The average individual is more likely to reject a partnership with someone who has a mental health disorder and also less likely to grant them a recommendation at work. Unsurprisingly, the people on the receiving end become hesitant to disclose their illness. The judgment of others is considered one of the greatest barriers to a satisfying life among people with a mental illness, as it blocks recovery and seriously diminishes their quality of life.
The psychological distress from discrimination and violence is linked to poor self-esteem along with anxiety and depression. These experiences can create barriers to social determinants of health like housing, employment, and education.
Research issues
The Canadian Mental Health Association (CMHA) has reported on the state of research into the connection between mental illness and violence, and their core finding is that no definitive causal relationship has been established.
A major problem with studies is that they fail to distinguish between various mental disorders, substance abuse, and co-occurring mental illnesses and addictions. The lack of standardization for what falls under "mental illness" means that different statistics can emerge depending on what disorders are left in or out of the study.
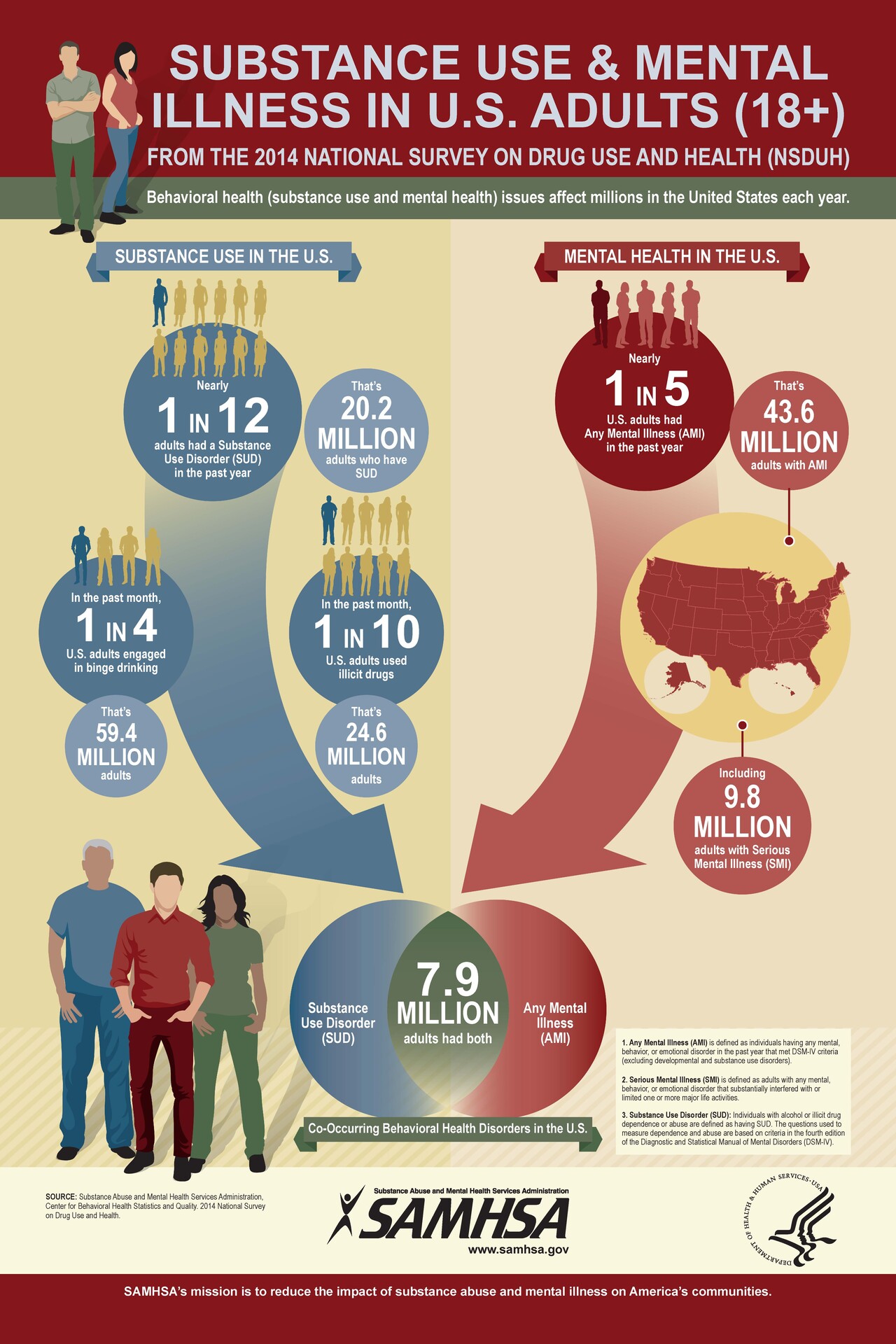
We have evidence showing that violent behavior is significantly more likely when a mental disorder co-occurs with substance use. But rates of violence for mentally ill folks who don't have a substance use issue are similar to that of the general population. This makes it hard to generalize research findings.
2016 research published in Clinical Psychological Science reported that once factors like feeling threatened, experiencing financial or marital distress, and substance abuse were removed, study participants were less likely to engage in violence than the general population.
Some studies use risk assessments to gauge an individual's likelihood of committing violence, but differences in methodologies and the types of risk calculations used lead us to different conclusions. You can find studies claiming bigger links between mental illness and violence and others that find no such relationship at all.
A Swedish study found that people with schizophrenia were 3.8 times more likely to be convicted for a violent crime than those without a mental disorder, but only 5% of all violent crimes could be attributed to mental illness across the country. Despite the raised odds, 19 out of every 20 violent crime convictions in Sweden were committed by someone without a mental disorder.
Psychiatric symptoms linked to violent behavior
Certain mental health symptoms can sometimes be drivers of aggression and violence, according to the American Psychological Association.
For people with psychotic disorders like schizophrenia, positive symptoms like persecutory delusions and command hallucinations can trigger violence. The former involves delusions where the patient feels they are being targeted, i.e., "someone is putting implants in my brain". Command hallucinations are the kind you hear of in the media, incidents where the patient was hearing voices that told them to harm someone.
Grandiose delusions, which manifest during the manic phases of bipolar disorder, have also been linked to violence. Patients can wildly exaggerate their own power and lose their ability to empathize with others in this state, creating conditions for a potentially aggressive encounter.
The intense energy of a manic state can be enough on its own. A 2014 study examining 429 crimes committed by 143 people with mental disorders found that 3% were directly related to depression, 4% to psychosis, and 10% to bipolar disorder. A youthful history of antisocial behavior is also connected to violence among those with a serious mental health disorder.
Interestingly, studies have also found that negative symptoms like apathy and a loss of motivation actually lower violence rates.
True drivers of violence
With so much attention poured on discovering the prevalence of violence among mentally ill people, not enough has gone to unearthing the causal factors of violence. The overarching determinants of violence are composed of demographic and socio-economic factors that can apply to anybody, mentally ill or not.
As stated by the World Health Organization and other bodies, being young, male, and of lower socioeconomic status are the leading factors in violent behavior. Other contributing factors include a history of experiencing or witnessing violence and involvement with the criminal justice system.
Life stressors of all kinds from job losses to grief, relationships breaking down, and traumatic experiences are strongly related to violence. Poor access to the resources we need to retain stability and health in our lives can also cause major stress, like poor housing, food, and income security, and unemployment. This circles back to what we already know about people with mental illnesses, who are highly susceptible to these situations.
The CMHA reports that people with serious mental illnesses are 3.7 times more likely to have been physically abused by their parents and 2.5 times more likely to be unemployed or to have seen physical fighting between parents than the general population.
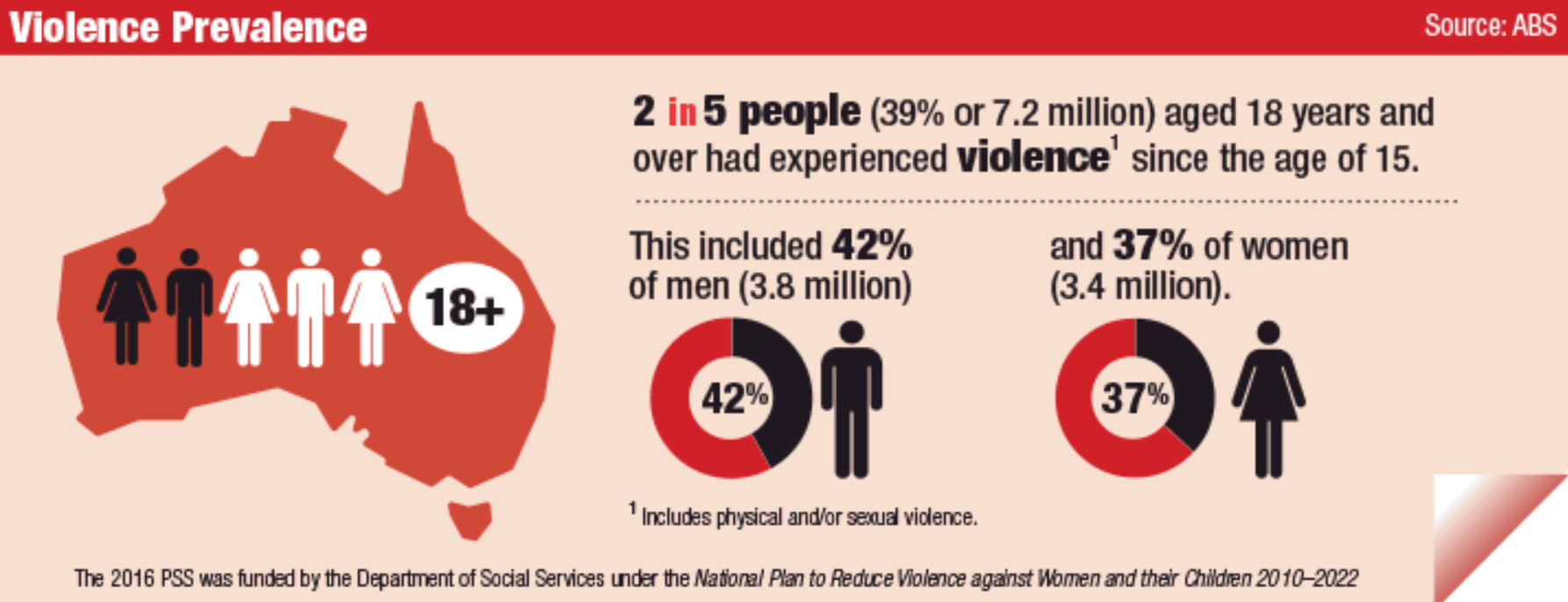
Seriously mentally ill people tend to be poorer and live in areas with higher crime rates, but poverty and bad social conditions are universal risk factors— not just for those living with mental illness. Regardless, we know what the headlines focus on when there's an incident. Violence begets violence, of course, and this is apparent across the board.
Neglect with services is an important part of the equation. A 2021 paper published by the Stanford Institute for Economic Policy Research found that, within two years of losing healthcare access, study participants with a history of mental illness were more likely to be jailed.
The author argued that extending the eligibility of Medicaid services would be a cost-effective way to reduce crime and related costs as well as keep more of these vulnerable people out of trouble. This is supported by a 2018 report by the Brookings Institute demonstrating how expanding access to healthcare lowers violent crime.